How your gut is controlling your immune system
By Lindzi Wessel
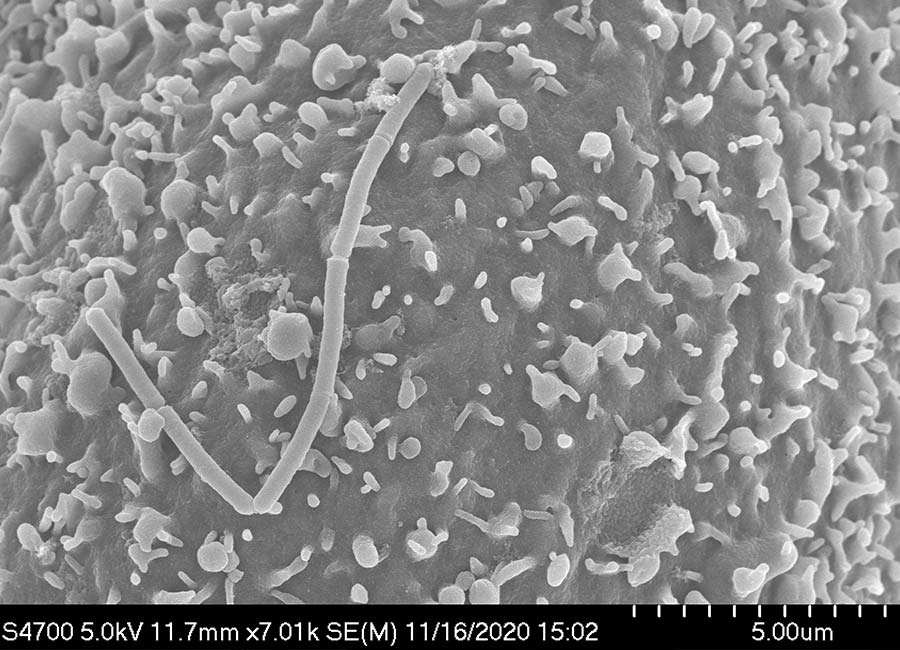
Microbes in the digestive system can affect the activity of our T-cells. CMIT scientists are exploring just how that happens.
As we grow and age in ways obvious to the naked eye, our immune system is changing too, developing and adjusting a delicate equilibrium to leave us with a discerning defense system. If this process goes well, our immune system is ready to wage war against dangerous invaders while standing down when confronted with the cells and tissue of our own body. A number of factors — like proteins in a mother’s milk or the production of sex hormones — likely come together to help establish this subtle balance. In recent years, health researchers have been increasingly exploring the role of one influencer in particular: bacteria in the gut.
Though the human microbiome is receiving more attention than ever before, scientists still know little about how the trillions of invisible hitchhikers on and inside of each of us might shape our immune responses. Now, a new study, by researchers from MIT’s Center for Microbiome Informatics and Therapeutics, offers important new clues by demonstrating how microbes from the human digestive system can direct the development of T-cells, a family of cells critical to immune function. The findings, published in Cell Host and Microbe, yield a better understanding of gut-immune “communication,” which experts hope might eventually mean help for patients with immune disorders for which few effective treatments currently exist.
“We are just at the tip of the iceberg in terms of understanding how gut bacteria and our immune cells talk to each other,” says Jun Huh, a CMIT Investigator and Associate Professor of Immunology at Harvard Medical School, who was one of the senior authors of the study. “But it’s like the first steps in deciphering a communication code between two kingdoms — we know it’s important and these early steps are very exciting.”
Offense, defense: The delicate dance of T-cell immunity
Crohn’s disease is an inflammatory disease affecting the digestive tract, which can lead to chronic pain and malnutrition and can sometimes be life threatening. Psoriasis is a condition that causes skin rashes and sometimes swollen joints. Type 1 diabetes occurs when a person’s pancreas ceases to produce insulin, disrupting the ability of cells to use sugar for energy. These distinct diseases have something critical in common: these conditions are all thought to result from the misbehavior of T-cells.
T-cells form in the bone marrow and, after an extended process of transformation in a small gland situated between the lungs, assume one of many roles in the immune system’s army. Some T-cells, like so-called Th17 cells, mount attacks against threats, secreting pro-inflammatory signals that round up other immune soldiers and sic them on pathogens. Others, like regulatory T-cells, do much the opposite, pumping the brakes when a battle isn’t needed.
“They are like the yin and the yang, with Th17 cells being pro-inflammatory and regulatory T-cells being anti-inflammatory,” says Huh. “Maintaining a fine balance between these T-cell subsets is very important.”
Losing that balance can have dangerous consequences. In psoriasis, for example, T-cells mistakenly target skin cells, driving a range of symptoms. In the inflammatory bowel diseases (IBD), Crohn’s disease and ulcerative colitis, out-of-control immune responses drive the degradation of the digestive tract. And T-cell disfunction is thought to play a role in other chronic diseases, like multiple sclerosis and rheumatoid arthritis.
Research into how we might wield control over T-cell behavior has thus become an important medical question. Only recently, though, have scientists started to understand how bacteria might be able to help.
A deep dive into digestive juices
An early clue that bacteria might help form the immune system came from “germ-free” mice — mice that live their entire lives in carefully controlled environments devoid of microorganisms. These mice consistently display T-cell imbalances and “don’t even develop Th17 cells,” says Sloan Devlin, a CMIT Research Faculty Member and assistant professor of Biological Chemistry and Molecular Pharmacology at Harvard Medical School. “It’s been known that differentiation of early T-cells into the various T-cell subsets is dependent on having a microbiome. But the mystery has been what’s the mechanism there.”
Devlin, who studies the human microbiome, has taken a particular interest in the importance of small molecules called bile acids and how they interact with bacteria in the gut. Bile acids are classified as natural “detergents” because they help us break down our food in much the same way soap helps get grime off the dishes. Sporting one “water-loving” and one “water-hating side,” both kinds of detergent bind to individual molecules of our meals and form balls around them, helping to pull one piece of food away from another in liquid. But viewing bile acids just as detergents is the “old school” way of thinking, Devlin says. Today, bile acids are being recognized more and more as signaling molecules that can influence the behavior of human cells, she says. And recent research from fellow CMIT Investigators points to a possible link between an individual’s unique mix of bile acids and their risk for IBD.
IsoalloLCA is a bile acid that, until recently, has represented little more than a detergent to the research community. But in 2019 Huh and colleagues found that isoalloLCA could increase the number of regulatory T-cells while another bile acid drove down the levels of Th17 cells. The study in mice made it clear that this long overlooked bile acid was important. But researchers still knew very little about it — they weren’t even sure where it came from. That changed when a postdoctoral scholar in Devlin’s lab, named Lina Yao, unexpectedly detected a high level of the bile acid in screens of bacteria sampled from human stool. IsoalloLCA, Yao realized, was being made by bacteria.
That discovery led to a series of experiments to determine just which bacteria were producing isoalloLCA. Working together, teams from Devlin and Huh’s lab identified a microbe from an abundant group of gut bacteria called Bacteroidetes that churned out isoalloLCA when the scientists provided it with the right ingredients. What’s more, the team found the Bacteroidetes genes that allowed the microbe to make isoalloLCA and figured out which human genes the bile acid acted upon to change T-cell activity. Then the team looked at the levels of isoalloLCA and Bacteroidetes genes in the microbiomes of a large sample of people and determined that missing Bacteroidetes and isoalloLCA from one’s microbiome was much more common among sufferers of ulcerative colitis and Crohn’s disease. The result clearly linked this gut bacteria to human disease via changes to the immune system.
“There’s a strong correlation between these factors and human disease,” Devlin says. “When you compare the people who are sick against people who are healthy, there’s a precipitous drop in the number of people who have this molecule and these bacteria”
From molecules to therapies
IsoalloLCA is likely not the only bile acid that is acting on the human immune system and Devlin, Huh and colleagues are now working to determine which others might also be important in T-cell development. Some of these molecules vary greatly in concentration from one person to another, suggesting the compounds could have wide ranging effects on human health. In fact, a Nature paper published by a group of investigators including CMIT Co-Director Ramink Xavier found that people who lived to be 100 years old or more had enriched levels of isoalloLCA in their microbiomes compared to the general population.
Though the teams of Devlin and Huh are excited by their new findings, the researchers caution that it’s too early for the results to drive concrete recommendations in terms of diet or probiotic consumption. “At this point we need to take it slow. These are just the first steps,” says Wei Li, a chemical biology graduate student in Devlin’s lab and co-first author on the paper.
There’s a lot of work left to be done, Devlin agrees. But, she says, “the exciting part” about having clearly identified the role of isoalloLCA and Bacteroidetes is that “once you have a small molecule identified, that’s a potential pathway towards a future treatment because that molecule can be developed as a drug. And if you have the important bacterial genes identified you could imagine how that might someday lead to a probiotic that makes this molecule. It’s a critical area to keep exploring.”

